Handoffs
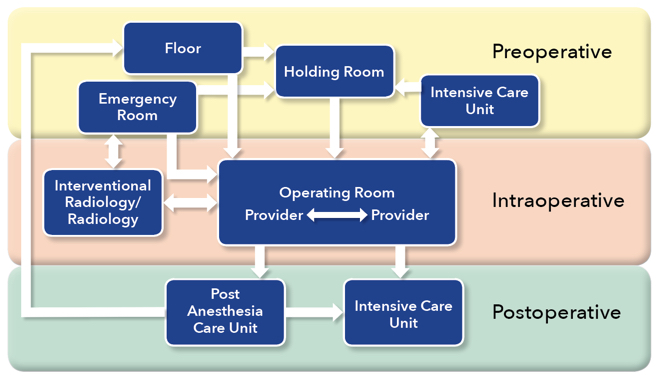
Handoffs (also referred to as “handovers”), in the most concise description, are an exchange of responsibility for one or more patients from one provider to another. Handoffs are “conversations rather than reports” 1 and typically consist of four phases – preparation (by both parties), patient arrival in the new location, the actual handoff (e.g., RN-MD interaction), and post-handoff management by the receiving clinician.2 The practice of perioperative care involves frequent transitions of patients between multiple areas. Well conducted handovers are critical for information exchange that enables relieving providers to provide care with hopefully the same factual and tacit knowledge of the patient as each and every previous provider. A handoff is an opportunity to review care and potentially correct mistakes; however, poor handovers may lead to information loss and adverse patient outcomes.3-5 Some of the major contributors to poor handovers include: distractions, interruptions, inadequate preparation, lack of a structured report, lack of understanding, production pressure, incomplete information exchange, and poor interpersonal interactions. The interactions between anesthesia providers and other medical professionals can be a source of a significant portion of all medical handoffs for a patient during their hospital course.
Preoperative
Holding Room to Operating Room
Most patients begin their operative course in a holding room, where they typically encounter preoperative nursing, anesthesia providers and their surgical team. The preoperative handoff thus begins in the holding room; yet, little information exists on these preoperative interactions. Holding room handovers usually involve information transfer between the patient or family member, a holding room nurse, an operating room (OR) nurse, and an anesthesia team member and may or may not include a surgical team member. The quality and content of the information communicated varies significantly.
Seven percent of anesthesia-related post anesthesia care unit (PACU) closed claims were related to preoperative preparation, and communication issues were classified as a contributing factor in 14% of the 419 recovery room incidents.4 The authors suggested that improvements in written, verbal and electronic transmission of information should be addressed. A pediatric preoperative handoff study, implemented a preoperative checklist that was associated with an improvement in 12 of 15 key items being discussed.6
Floor/Emergency Room/Intensive Care Unit to Operating Room
Patients do not always arrive to the OR from a holding room. They may come to the OR from any number of locations, such as the emergency department, medical floor or intensive care unit (ICU), either directly or via the holding room. The variability in culture in these locations presents its own challenges and barriers, as each location may have different preparation techniques prior to OR transfer. Team composition, policies, charting and methods of communication may differ from unit to unit. In addition, there may be limited information available due to the emergent nature of some procedures. In a study of neonatal intensive care unit (NICU) to OR handovers, several barriers to information exchange were discovered.7 These included lack of a standardized report, patient not prepared for transfer, unclear transition of care between team members, unclear provider roles, significant provider traffic in and out of the room, and distractions or interruptions. Not only do the providers present at the time of handover vary widely, but up to 10 different providers may be present at any given handover. In addition, the perception of handover quality varied widely between NICU providers (MDs, RNs, NPs) and anesthesia providers (MDs, CRNAs, RNs), with 41% reporting “fair” to “poor” and only 35% reporting “very good” to “excellent”. Caruso showed that standardizing ICU to OR handoffs increased communication without delaying surgery and improved anesthesia provider satisfaction scores.8
One study, which followed 20 patients from the ward through their surgical course, found that the pre-procedural teamwork phase had the largest amount of failures (61.7%).9 Although the anesthesia team had 86.6% of necessary preoperative information and the surgical team had 82.9% of necessary information, the nursing team only had 25% of the total information and only 27% of the total information was known by all primary team members (surgeon, anesthetist, surgical assistant, scrub tech, and circulating nurse). Verbal handover from the ward to the OR team only occurred in 43% of the patients and in 10% of the cases there was no communication between the ward nurse and the OR team receiving the patient. They reported that information transfer failures contributed to a total of 18 incidents and adverse events in 15 out of 20 patients. In another study by Nagpal, three types of information transfer and communication failures were described in the preoperative phase:10 source failures (information at different places, consents missing, inadequate documentation), transmission failures (lack of communication between anesthesia and surgical teams, lack of communication between the ward and OR staff, information not relayed), and receiver failures (specialists’ opinions not followed, checklists not followed). These failures had effects on patients, teams and the organization (such as case cancellations, provider stress and wastage of resources) but these effects were not linked to any particular phase of failure.
Intraoperative
Provider-Provider
To our knowledge, only a handful of studies exist on intraoperative handoffs. Handoffs between all anesthesia providers may be for short duty relief breaks or shift to shift relief. However, their presence may be associated with quantifiably increased morbidity and mortality,11 and the association strengthens with each additional handoff. On the other hand, there may be a benefit associated with intraoperative handoffs, in that they may bring a fresh set of eyes to discover issues and errors.3
The intraoperative environment must be considered a part of the transition from preoperative to postoperative care, and handovers within that setting should be treated similarly. However, the intraoperative handoff is often rushed, conversational, and not at all structured. The entirety of the perioperative course may benefit from improved structured communication,12 and the intraoperative course is no exception. The quality of intraoperative handovers has substantial variability,13 depending on location, setting, and culture. Structured handovers in a pediatric population have resulted in significantly decreased communication errors and increased reliability and effectiveness of communication in the operating room.14 Agarwala also found that an electronic checklist improved relay and retention of critical information and clinician information at intraoperative handoff of care.15
Location/Procedure Change
Some situations require a change in location and staff due to surgical issues or needs. For example, some institutions provide multiple anesthetics for multiple procedures at multiple locations on a single infant or child to minimize the number of exposures to general anesthesia.16 At other times, patients may require additional testing during an anesthetic such as interventional or radiological imaging as part of a surgical procedure. In addition, a second operative team may take part in the procedure, and their presence at the initial handoff or time-out is unlikely to be consistent.
These changes in procedure and location lead to multiple handoffs between anesthesia, surgical, nursing and technical staff, and often require additional team members who may not have been part of the initial preoperative handoff and therefore, will likely have limited information regarding the patient. These handoffs inevitably add complexity to the procedural care of the patient. Strategies to manage the increased complexity include an additional time-out when a new team assumes care of the patient, recounting of instruments and supplies, and mandatory surgical site imaging post-procedure. Regardless of the strategy, providers must recognize these changes as handovers of care.
Postoperative
Operating Room to Post Anesthesia Care Unit
Postoperative handoffs are the most common and most studied handovers in the field of anesthesiology. These typically involve anesthesia staff providing report to PACU nursing staff and may also involve surgical team members. In studies of routine postoperative handovers, it was found that significant amounts of information were frequently missed, such as ASA status, antibiotics received, and fluid management.17 Handoffs of ambulatory patients also commonly resulted in omission of data and resulted in poor receiver satisfaction.18 Composites of overall handoff quality are judged to be “good” less than half of the time following patient delivery to the PACU19 and the variable quality of communication of pertinent case events in most postoperative handovers is associated with a perceived increase in complication rate.13,20 With regards to claims data, 14% of anesthesia-related PACU issues were attributed to failures or deficiencies in communication.4
As noted above, structured handovers in a pediatric population have significantly decreased communication errors and increased reliability and effectiveness of communication in the OR, and also in the PACU.14 Nagpal also reported a decrease in information omission and task errors and an increase in staff satisfaction after institution of a standardized handoff tool.12 One study showed that a multimodal intervention substantially improved PACU handoffs and the effect continued to be present 3 years after the intervention.21 Overall, the data available supports the use of a structured approach to postoperative handoff that includes a tool and education about its use.
Operating Room to Intensive Care Unit
OR to ICU handoffs often include anesthesiology and surgical team members, OR nursing, and ICU team members which may include physicians, nurse practitioners, physician assistants, nursing staff, respiratory therapists and others. In some cases, the handoff from the operating room to the ICU may be the first structured handoff in a patient’s hospital course, especially in emergency situations. Although many of these studies have limitations, standardized ICU handovers may be associated with reduced long term ICU complications.22
Improvement in the safety and quality of handovers of patients from surgery to the intensive care unit may occur through the adoption of the Formula 1 pit stop/aviation structured approaches.23 Zoccoli et al. also reported the perception of improved consistency of data shared during handovers and an increase in interdisciplinary communication by nursing staff following institution of a standardized handover tool in the surgical intensive care unit.24 The most robust data on improving OR to ICU handover processes has taken place in the cardiovascular ICU. However, it is clear that other care environments require further studies to clarify the optimal way by which to perform a patient handoff.
Summary
While much of the data regarding handoffs and outcomes has been generated from postoperative and a few intraoperative exchanges, many of the barriers to effective communication exchange are universal, such as patient complexity, distractions, provider fatigue, time constraints, multi-tasking and situational awareness/appreciation for different roles.25 Additional work in this area would likely improve understanding of these deficits and improve patient safety and provider satisfaction.
References
- Lane-Fall MB, Brooks AK, Wilkins SA, Davis JJ, Riesenberg LA. Addressing the mandate for hand-off education: a focused review and recommendations for anesthesia resident curriculum development and evaluation. Anesthesiology. 2014;120(1):218-229a.
- Segall N, Bonifacio AS, Schroeder RA, et al. Can we make postoperative patient handovers safer? A systematic review of the literature. Anesthesia and Analgesia. 2012;115(1):102-115.
- Cooper JB, Newbower RS, Long CD, McPeek B. Preventable anesthesia mishaps: a study of human factors. Anesthesiology. 1978;49(6):399-406.
- Cooper JB, Long CD, Newbower RS, Philip JH. Critical incidents associated with intraoperative exchanges of anesthesia personnel. Anesthesiology. 1982;56(6):456-461.
- Cooper JB. Do short breaks increase or decrease anesthetic risk? Journal of Clinical Anesthesia. 1989;1(3):228-231.
- Arbous MS, Meursing AEE, Van Kleef JW, et al. Impact of anesthesia management characteristics on severe morbidity and mortality. Anesthesiology. 2005;102(2):257-268.
- Saager L, Hesler BD, You J, et al. Intraoperative transitions of anesthesia care and postoperative adverse outcomes. Anesthesiology. 2014.
- Hyder JA, Bohman JK, Kor DJ, et al. Anesthesia care transitions and risk of postoperative complications. Anesthesia & Analgesia. 2016;122(1):134-144.
- Hudson CCC, McDonald B, Hudson JKC, Tran D, Boodhwani M. Impact of anesthetic handover on mortality and morbidity in cardiac surgery: A cohort study. Journal of Cardiothoracic and Vascular Anesthesia. 2015;29(1):11-16.
- Terekhov MA, Ehrenfeld JM, Dutton RP, Guillamondegui OD, Martin BJ, Wanderer JP. Intraoperative care transitions are not associated with postoperative adverse outcomes. Anesthesiology. 2016;125(4):690-699.
- Hyder JA, Bohman JK, Kor DJ, et al. Anesthesia care transitions and risk of postoperative complications. Anesthesia & Analgesia. 9000; Publish Ahead of Print.
- Agarwala AV, Firth PG, Albrecht MA, Warren L, Musch G. An electronic checklist improves transfer and retention of critical information at intraoperative handoff of care. Anesthesia & Analgesia. 2015;120(1):96-104 110.1213/ANE.0000000000000506.
- Boat AC, Spaeth JP. Handoff checklists improve the reliability of patient handoffs in the operating room and postanesthesia care unit. Paediatric Anaesthesia. 2013;23:647-654.
- Jullia M, Tronet A, Fraumar F, et al. Training in intraoperative handover and display of a checklist improve communication during transfer of care. European Journal of Anaesthesiology. 2017;34(7):471-476.
- Weinger MB, Slagle JM, Kuntz AH, et al. A multimodal intervention improves postanesthesia care unit handovers. Anesth Analg. 2015;121(4):957-971.
- Joy BF, Elliott E, Hardy C, Sullivan C, Backer CL, Kane JM. Standardized multidisciplinary protocol improves handover of cardiac surgery patients to the intensive care unit. Pediatric Critical Care Medicine. 2011;12(3):304-308.
- Catchpole KR, De Leval MR, McEwan A, et al. Patient handover from surgery to intensive care: Using Formula 1 pit-stop and aviation models to improve safety and quality. Paediatric Anaesthesia. 2007;17(5):470-478.
- Craig R, Moxey L, Young D, Spenceley NS, Davidson MG. Strengthening handover communication in pediatric cardiac intensive care. Paediatric Anaesthesia. 2012;22(4):393-399.
- Agarwal HS, Saville BR, Slayton JM, et al. Standardized postoperative handover process improves outcomes in the intensive care unit: A model for operational sustainability and improved team performance. Critical Care Medicine. 2012;40(7):2109-2115.
- Kaufman J, Twite M, Barrett C, et al. A handoff protocol from the cardiovascular operating room to cardiac icu is associated with improvements in care beyond the immediate postoperative period. Joint Commission Journal on Quality and Patient Safety. 2013;39(7).
- Patterson ES, Roth EM, Woods DD, Chow R, Gomes JO. Handoff strategies in settings with high consequences for failure: Lessons for health care operations. International Journal for Quality in Health Care. 2004;16(2):125-132.
- Starmer AJ, Spector ND, Srivastava R, et al. Changes in medical errors after implementation of a handoff program. New England Journal of Medicine. 2014;371(19):1803-1812.
- Keebler JR, Lazzara EH, Patzer BS, et al. Meta-analyses of the effects of standardized handoff protocols on patient, provider, and organizational outcomes. Human Factors: The Journal of the Human Factors and Ergonomics Society. 2016.

