When developing a curriculum to expand training in handoffs, simulation-based learning can be an attractive option that balances psychological safety and realism for the trainee.1,2 We have outlined some best practices below and offered some recommendations for making the most of the experience for your learners.
First, it is important to understand the background and training of your audience. Factors such as the clinical background, training level, practice environment, and previous simulation experience can have a major impact on the success of your program. Here are some guidelines to consider:
Undergraduate: Regardless of training progress, these learners will benefit from dedicated pre-briefing time, clear explanations of simulation capabilities (e.g. what information is available and what they may request).
- Pre-clinical/early clinical: Less experienced learners benefit the most from prework that provides clinical orientation. The group tends to respond well to distilled summaries of required knowledge (written) and video (live or animation) that can easily be adapted to virtual or distance learning experiences.
- Clinical learners: Work to maximize direct interactions with professional or near professional facilitators (residents, advanced learners) through learner specific debriefs. This helps the learner orient to the utility of the task in practice.
Graduate, resident, and early career: Tactile and/or in situ learning environments can produce robust satisfaction and achievement of learning objectives. Consider dedicated training for debriefers in preparation of simulation days.
Continuing and professional education: While responsive to advanced techniques via direct learning, the flexibility of online or virtual courses makes it adaptable to diverse clinical schedules. Always enable prework to be multimodal in order to address differences in learning preferences.
Next, plan a suitable practice environment for the simulation.3 When possible, having multiple professions take part to reflect in a simulation offers a more accurate, real-world scenario. This enhances the value of any exercise, yet often requires additional scheduling and logistical work. Then consider the level of reality that your particular simulation environment can reflect.
High Fidelity |
|
In situ
|
|
Simulation rooms
|
|
Patients vs. Doll
|
Low Fidelity |
|
Online or distance learning
|
|
Serious games
|
|
Virtual reality
|
Finally, consider the resources necessary for your learners to succeed. Some audiences will prefer certain formats over others, but a well-structured introduction can greatly increase the effectiveness of the session:
- Introduce purpose and format of event
- Provide overview of any learning needed as groundwork
- Set expectations for evaluation and feedback
We applied many of the above concepts while designing and optimizing courses to introduce handoff education into our undergraduate medical education. Termed the Quality Enhancement Plan (QEP) – Team FIRST, our project aims to bolster competencies in teamwork and communication by developing a longitudinal curriculum for health professions and medical students.4 At baseline, these simulated activities utilized participant feedback as important source material for continued course improvement. However, qualitative comments can be challenging to compile and consolidate into clear theme for course improvement unless an established approach is applied.
To best quantify and prioritize participant and facilitator comments, we apply principles of quality functional deployment (QFD) in the form of focus groups to collect relevant feedback. We took these comments and used affinity sorting to distill the most frequently mentioned elements in each focus group session (Figure 1).
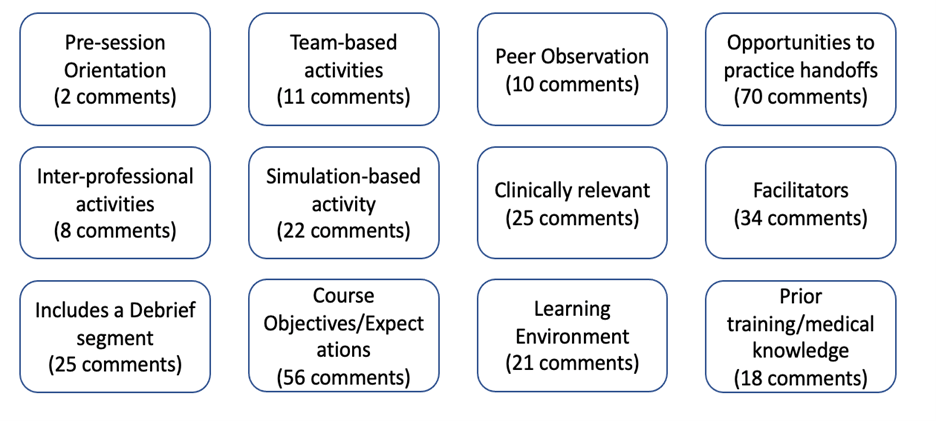
Focus group participants write down individual comments regarding various aspects of each simulated activity on sticky notes. The research team then collects these comments and individually sorts comments into broad categories. Finally, we compare our rough categories to identify the student and faculty needs for each simulation activity.
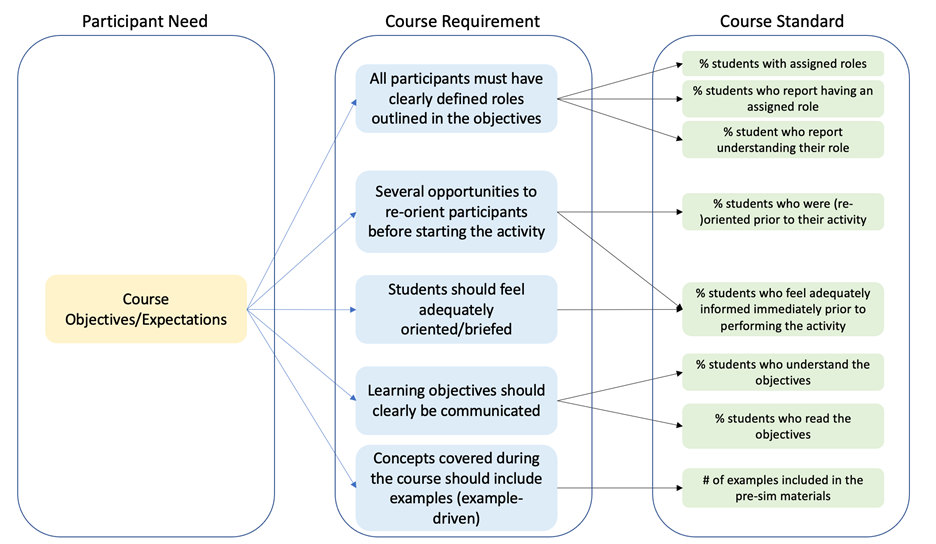
Next, we utilize a critical to quality (CTQ) tree to identify requirements to focus our quality improvement efforts for course improvement (Figure 2). Interestingly, when building our CTQ tree, many of the derived requirements mirror the current literature covering simulation education. For example, “setting expectations for evaluation ahead of the simulation” was a requirement we frequently identified in several of the handoff activities.
Once participant needs are isolated, we placed each one into a critical to quality (CTQ) tree. These needs drive future items that must be included in each simulated activity (course requirements). Lastly, we identify quantifiable approaches to measure each requirement, ensuring that each future participant feels that the requirement is present in the course. Here we show the CTQ tree for just one of the needs identified.
We will continue to optimize the use of simulation to advance competencies in teamwork and communication over the course of this 5-year project funded by the UT Southwestern Office of Medical Education. Our evidence-based approach underscores the importance of incorporating focus group-mediated feedback as the “voice of the customer” (students) using it as a means for improving the effectiveness of simulation-based education.
References
1. Au K, Lam D, Garg N, et al. Improving skills retention after advanced structured resuscitation training: A systematic review of randomized controlled trials. Resuscitation. 2019;138:284-296.
2. Lorello GR, Cook DA, Johnson RL, Brydges R. Simulation-based training in anaesthesiology: a systematic review and meta-analysis. BJA: The British Journal of Anaesthesia. 2014;112(2):231-245.
3. Kurup V, Matei V, Ray J. Role of in-situ simulation for training in healthcare: opportunities and challenges. Current Opinion in Anesthesiology. 2017;30(6):755-760.
4. The University of Texas Southwestern Medical Center: Quality Enhancement Plan for the Southern Association of Colleges and Schools Commission on Colleges. The University of Texas Southwestern Medical Center;2019.


