Most of us in healthcare can attest to quality improvement (QI) projects that have come and gone. Too many of us who work in QI lament the projects that we poured our blood, sweat, and tears into only to have their initial benefit disappear over the course of a few years. The initial enthusiasm wanes, the staff turns over, and improvement in patient safety is lost. Time and again, we see improvement in metrics after the QI project has been rolled out, but sustained change is tougher. What is it that makes some changes sink in and stick while others fail? And what can we learn from efforts that have sustained improvement over a longer period?
The field of implementation science aims to address these questions. In the inaugural issue of Implementation Science, Eccles and Mittman, define the field as “the scientific study of methods to promote the systematic uptake of research findings and other evidence-based practices into routine practice, and, hence, to improve the quality and effectiveness of health services. It includes the study of influences on healthcare professional and organizational behavior.” [2] Implementation science improves patient care by effecting the systematic uptake of research findings and evidence-based practices across medical specialties, healthcare disciplines, and types of institutions. Its application includes motivating behavior changes in both healthcare providers, as well as patients.
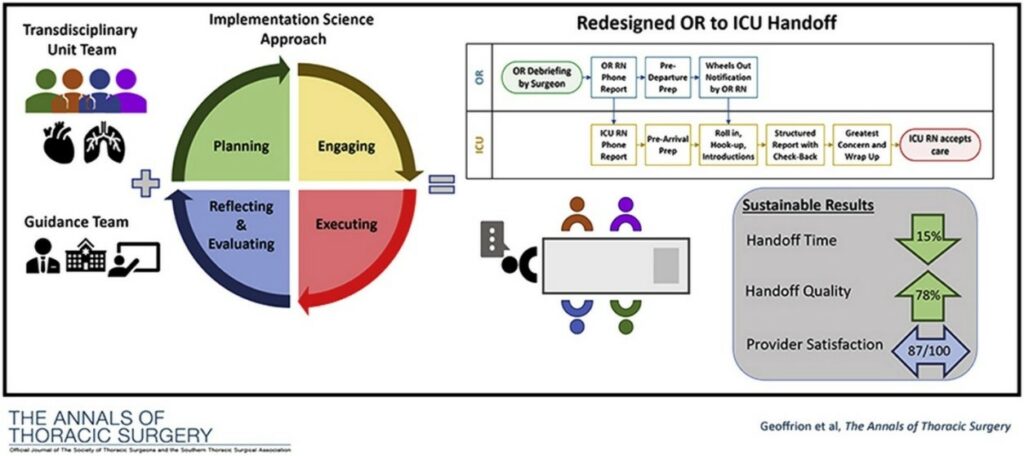
Geoffrion and colleagues, including MHC’s own Isaac Lynch and Philip Greilich, studied an implementation science approach to handoff redesign in the cardiac surgery ICU. [1] In this study, the authors formed the ECHO-ICU (Enhanced Communication during Handover from OR to ICU) team and used a twelve-step implementation process, summarized in the figure below, to collectively redefine and develop an “ideal” handoff process from the cardiac OR to the Cardiovascular ICU (CVICU). The ECHO-ICU project was supported by a guidance team including a physician quality officer, a project manager, a nurse coordinator, a data analyst, and subject matter experts in human factors, ergonomics, and quality improvement. Their team developed a handoff improvement bundle (including team training, standardized education, video illustration, and cognitive aids) that was implemented over a one-year period.

PDSA, plan-do-study-act; QI, quality improvement); Source: Geoffrion, et al. [1]
Adherence to 57 handoff best practices was assessed with video recordings of post-operative handoffs in the 18 months before and after the implementation period. Improvement in 23 best practices was observed in the post-implementation period, while 17 were preserved, 15 were unaffected, and 2 were reduced. Importantly, improvement in 13 best practices deemed most valuable was sustained 2.5 years following implementation. Additionally, overall patient outcomes were studied pre- and post- implementation of the handoff bundle, and demonstrated a lower rate of prolonged mechanical ventilation and a shorter length of stay after the bundle was implemented.
The approach taken by the ECHO-ICU team echoes what we have learned about successful implementation from the business world and from other quality improvement examples in healthcare. John Kotter, a Professor of Leadership Emeritus at Harvard Business School, described an 8-Step Process for Leading Change based on decades of observations of leaders and organizations who were successful in executing transformational change. [3] From their initial planning stage onward, the ECHO-ICU team incorporated many of these elements into their work, including the building of a guiding coalition of their operational and executive leaders and the formation of a strategic vision and initiatives. I-PASS is another example of implementation science at work in healthcare. I-PASS is evidence-based handoff bundle, initially piloted amongst pediatric residents in pediatric medical-surgical units, which leveraged Kotter’s model of transformational change. [4] I-PASS embraced Kotter’s techniques of creating and communicating a clear vision for their transformation, celebrating short-term wins, and institutionalizing new approaches. ECHO-ICU begins to bring to the perioperative realm what I-PASS accomplished in the inpatient arena.
Implementation of emergency manuals is another area of multidisciplinary patient safety efforts in perioperative medicine, and one from which we can learn more about the factors that lead to implementation success. Aladina and colleagues conducted a cross-sectional study of factors influencing successful implementation of OR emergency manuals, and found that centers who had completed more implementation steps had a 50% higher odds of successful implementation. Additional factors that were associated with implementation success include leadership support and dedicated time for staff training. [5] With this experience in mind, it comes as no surprise that the ECHO-ICU study realized not only short-term, but sustained improvement through their structured implementation plan, early incorporation of a transdisciplinary unit team and a leadership guidance team, and team training using standardized educational materials.
The ECHO-ICU study demonstrates that a structured and strategic approach to implementation can not only be successful, but it can engrain the improvement in our culture and lead to lasting transformation. The lessons we take from ECHO-ICU are ones that can be replicated at other centers, not only in handoff improvement, but also in other domains affecting perioperative patient safety and quality. What can certainly be concluded is that change cannot occur in a vacuum; it takes cohesive efforts across disciplines and commitment by our leaders. The MHC is moving forward in equipping our member organizations and perioperative clinicians everywhere with the implementation tools, like those used in ECHO-ICU, needed for success.
References
1. Geoffrion, T.R., et al., An Implementation Science Approach to Handoff Redesign in a Cardiac Surgery Intensive Care Unit. Ann Thorac Surg, 2020. 109(6): p. 1782-1788.
2. Eccles, M.P. and B.S. Mittman, Welcome to Implementation Science. Implementation Science, 2006. 1(1): p. 1.
3. Kotter, J., Leading Change. 1996, Boston, MA: Harvard Business School Press.
4. Rosenbluth, G., et al., I-PASS Handoff Program: Use of a Campaign to Effect Transformational Change. Pediatr Qual Saf, 2018. 3(4): p. e088.
5. Alidina, S., et al., Factors associated with the use of cognitive aids in operating room crises: a cross-sectional study of US hospitals and ambulatory surgical centers. Implement Sci, 2018. 13(1): p. 50.


